Dear readers,
If you are an ACNM (American College of Nurse Midwifery) member, please access and sign the open letter supporting the provision of trans health as a core competency for nurse midwives by clicking the link below.
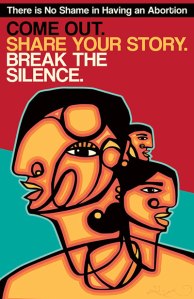
The letter captures so many sentiments I share about why trans healthcare should be absolutely integrated into nurse midwifery from the beginning. Let’s stop ghettoizing any reproductive healthcare (including miscarriage management, elective abortions, basic assisted reproductive therapies for LGBT clients) — and in this moment, especially trans affirming care — and respond to the fact that queer and trans midwives and clients are demanding an expansion of core care that is appropriate and respectful. And let’s please root out the gender essentialism and transphobia in the midwifery community and the current ACNM leadership! Thank you to all the wonderful folks who put together this letter and who have been working so hard to advance an intersectional feminist leadership in midwifery. Our side will prevail.
-A proud signer to this letter and member of The Queer and Transgender Midwives Association (QTMA)
*********************
As ACNM members, we submit this letter to raise our concerns about the ACNM Board of Directors’ (BOD) recent actions in making decisions about access to care for transgender and gender non-conforming (TGNC) people in closed session and without any mechanism for transparency or accountability. We submit this letter on Transgender Day of Remembrance in the spirit of honoring the lives of those we have lost to transphobia, and fighting for the rights of those who continue to survive. We are publishing this letter publicly so that midwives and midwifery students can sign on in solidarity.
We are alarmed to learn that at their October 2018 Board meeting, the newly-elected BOD 1) failed to approve proposed revisions to the ACNM Position Statement on care of TGNC people, and 2) failed to uphold the March 2018 decision of the previous BOD, which had confirmed that the midwifery core competencies as they currently stand already include gender affirming hormone therapy for TGNC people. Instead, the BOD rejected the Position Statement, stating that “neither hormone therapy or care of natal men [sic] is a core competency.”
These actions were motivated by concerns regarding midwifery care of transgender women and non-binary people assigned male at birth (referenced by the BOD as “natal men”), and are in direct opposition to the recommendations of the Gender Equity Task Force (GETF) Chair and the Core Competencies Committee Chair. No midwives who identify as TGNC or who provide care to TGNC communities participated in the closed discussions related to these motions.
Frustratingly, the BOD is able to withhold the detailed minutes of their discussion per protocol that only open session minutes are released publicly. The BOD included only very vague information on this discussion in the open session minutes. This is particularly concerning given that these BOD decisions have significant implications for work currently underway by the GETF and a number of ACNM committees. In reviewing the available open session notes, it is notable that the only topics from open session that were moved to closed session were related to midwifery care of TGNC people.
With this letter, we intend to alert the BOD and ACNM’s membership of:
- The presence of the many current and future midwives who stand in support of transgender, non-binary, gender-diverse and intersex people;
- The importance of midwifery care for these communities;
- The ethical implications of the BOD’s lack of transparency; and
- The practice implications of these decisions on us all.
The BOD’s actions are very concerning in that they create an impression that gender affirming hormone therapy – widely recognized as straightforward and lifesaving care – is not appropriate for new-to-practice midwives. This creates a barrier to increasing the number of providers equipped to provide this care, a development that is very problematic given the significant and well-documented health disparities experienced by TGNC communities. It is important to remember that midwives – including new midwives – are well versed in many forms of hormone therapy (such as for contraception and for management of menopausal symptoms), and that these other therapies are uncontested in their inclusion in the core competencies. Therefore, the BOD’s exclusion of only gender affirming hormone therapy specifically and unethically targets TGNC people.
While we cannot presume to know the exact intent of BOD members participating in these decisions, the impact is clear. These decisions are transphobic; they send a message that the current BOD does not view transgender women as “real women” simply because some transgender women have a penis; otherwise they would be deemed inherently appropriate for midwifery care under the ACNM vision of “a midwife for every woman.” Importantly, midwives are able to care for people with penises when it comes to circumcision, as part of expanded midwifery practice. Thus, these motions are clearly not an issue of scope, but of what ACNM leadership finds uncomfortable politically or personally.
The BOD did not specifically state concerns regarding midwifery care of transgender men and non-binary people assigned female at birth. In more neutral circumstances this could be perceived as reassuring or benign. However, in the context of the BOD’s actions it raises concern that the BOD perceives transgender men as “women” regardless of their gender identity, simply because some of these individuals may have breasts, ovaries, a uterus, and a vagina. This negates the true selves and humanity of these individuals, and tarnishes the value of midwifery care by filtering care provision through a lens of transphobia.
Biological determinism, the act of reducing a person’s identity to their body parts, is inhumane, abhorrent, and unconscionable. This is the first time the BOD has attempted to make any distinctions between TGNC individuals based on anatomy. Previous BODs have intentionally described TGNC care inclusively, recognizing that gender is a spectrum and that anatomical distinctions reinforce biological determinism. Our peers in allied professions which have historically defined their scope of practice as “care of women” (Obstetricians/Gynecologists and Women’s Health Nurse Practitioners) have long affirmed that care of all TGNC people – including transgender women – is important and within their scope. Our own prior BOD did the same in March of this year. Yet the current BOD has decided to change course entirely, in a move that favors biological determinism and is particularly foreboding given the current political climate.
Within the past month, the Department of Health and Human Services released a memo stating that it is planning to require that gender be identified as a biological condition determined by genitalia at birth. Immediately, over 2,600 experts in the field, including both scientists and care providers, published a response, stating that to define someone by genitalia is “not only fundamentally inconsistent with science, but also with ethical practices, human rights, and basic dignity.” Why are we, as a profession, reversing our prior well-thought-out decisions and joining in a widespread assault on the rights, bodies, and health of transgender and non-binary people? Why have we sided with anti-science and transphobic positions by defining who midwives can take care of based on their genitals alone?
This position places midwives in the inappropriate position of acting as “gender police” tasked with determining who is “woman enough” to receive midwifery care, and leaves the many midwives already providing sexual and reproductive healthcare to gender diverse patients in professional and licensure limbo. Given research that indicates people of color are more likely to identify as TGNC than their white counterparts, limiting access to care for TGNC people also serves to further the already significant health disparities experienced by communities of color.
The truth is that midwives take care of people, not body parts, and that body parts are not inherently gendered. As midwives we pride ourselves on treating the whole person. We care holistically, we believe what people tell us, and we meet patients where they are. These BOD decisions are ethically in conflict with core midwifery values. Instead of providing guidance for clinicians, they require that we choose between practicing midwifery, and participating in a political decision by our professional organization that privileges bigotry and ignorance over the people harmed by that bigotry. They violate midwifery’s ethical obligations as care providers and reinforce the systemic oppressions already experienced by TGNC and intersex people. They use midwifery as a tool to amplify harm rather than increase equity. That is not acceptable.
We will not stand by as this BOD makes decisions that dehumanize the patient populations we are honored to serve. We will not stand by as this BOD makes decisions that dehumanize our own midwife colleagues who are TGNC or intersex.
We ask the BOD to do the following:
- Commit to holding all future discussion of this issue in open session;
- Reinstate the March 2018 decision that care of TGNC individuals and provision of gender affirming hormone affirmation therapy falls within entry midwifery care as outlined in the Core Competency document Section V.C.
- Approve the revised Position Statement and revised Core Competencies documents as submitted by the GETF to the BOD for the October 2018 meeting, without the addition of restrictions on the care of transgender women or the provision of gender affirming hormone therapy
- Charge the GETF and other relevant ACNM Volunteer Committees to work collaboratively to review and update the Midwifery Scope of Practice document to include care for TGNC individuals.
- Publicly acknowledge the damage that has been done by the BOD’s recent actions, and outline a plan for accountability in the future, including BOD and DOME additional training in gender diversity and impact on health disparities.
- Use respectful and inclusive language when referring to TGNC individuals and communities in all communications and public documents; guided by ACNM’s Issue Brief on “Use of Culturally-Appropriate Terminology for Gender-Diverse Populations
- Charge the Ethics Committee to review public documents that have potentially political implications.
We, as individuals deeply committed to increasing healthcare access to TGNC populations, hope that you will join us as we continue to strive towards a more inclusive path for midwifery. These signatures below affirm and signify the gravity of the harm we feel these decisions have brought forth by excluding vulnerable individuals from midwifery care.
We invite you to consider taking the following steps:
- Signing this letter in support of inclusion of midwifery care for all bodies;
- Sharing this letter with peers, friends, colleagues, and students;
- Educating people about affirming language and engaging in conversations in a way that supports all people;
- Sending a personalized letter to a regional representative or the BOD;
- Running for office, and/or intentionally supporting the leadership of TGNC midwives in regional and national leadership roles, so that we have a Volunteer structure that understands TGNC issues;
- Sending a letter to your current midwifery Director or the Director at your Alma Mater, with copies to DOME, to advocate for the inclusion of this education in midwifery programs.
For midwives and midwifery students who are TGNC and LGBQ identified: The Queer and Transgender Midwives Association (QTMA) is dedicated to supporting and representing LGBTQIA2S+ midwives and student midwives as they train and grow as providers and people. QTMA provides educational opportunities, advocacy, community and tools for their members, all grounded in an intersectional ideology and framework. It envisions a world where all LGBTQIA2S+ midwives and student midwives have the resources and representation they need to thrive in practice and in their community. QTMA is fiscally sponsored by the birth justice organization, Elephant Circle. Interested folks can connect with QTMA on their Facebook page or by emailing QTmidwives@gmail.com.
Sincerely,
Stephanie Tillman (she/her), CNM, University of Illinois, Region IV – Chair, ACNM Gender Equity Task Force
Simon Adriane Ellis (they/them, he/him), CNM, Kaiser Permanente Washington, Region VII – Member, ACNM Gender Equity Task Force
Noelene K. Jeffers, (she/her), CNM, Region II, Member, ACNM Gender Equity Task Force
Margaret Haviland (she/her), CNM, WHNP-BC, Kernodle Clinic, Region III, Member – ACNM Gender Equity Task Force
Signey Olson (she/her), CNM, WHNP-BC, Columbia Fertility Associates, Region II – Member, ACNM Gender Equity Task Force
Lily Dalke (she/her), CM, LM, Planned Parenthood NYC, Region I – Member, ACNM Gender Equity Task Force; Member, ACNM Core Competencies Committee
Nikole Gettings (she/her), CNM, Region III- Member, ACNM Gender Equity Task Force
Anne Gibeau (she/her/hers), CNM, PhD, Director of Midwifery – Midwifery Practice, Jacobi Medical Center, Region 1, New York State Association of Licensed Midwives – Downstate Region Representative; Member – ACNM Gender Equity Task Force
Máiri Breen Rothman (she/her), CNM, MSN, FACNM, Director, M.A.M.A.S., Inc., Region II; Member – ACNM Gender Equity Task Force
Meghan Eagen-Torkko (she/her), PhD, CNM, ARNP, University of Washington Bothell and Public Health Seattle-King County, Region VII — Member, ACNM Ethics Committee
Lee Roosevelt (she/her), PhD, MPH, CNM, University of Michigan, Region IV
Jenny Nelson, (she/her), CNM, Region I
Jennifer M. Demma (she/her) MSN, APRN-CNM, Family Tree Clinic, Region V
Rob Reed (they/them), CNM, ARNP, IBCLC, Swedish Medical Center, ACNM Region VII – WA ACNM Affiliate Vice President
https://docs.google.com/document/d/1jS9Mxdkh45ROZR38H0yXYVI2Bxh05v6aZhCy0u0m57A/edit?usp=sharing